Stroke Recovery
At the Bayview Stroke Intervention Clinic (BaSIC), patients are seen for follow-up at 1, 6, and 12-months post-infarct. Many of these patients have relatively small strokes, as shown on the right image in these brain MRI scans. Patients with a stroke of this size typically lack major motor and language impairments and can appear as though they are fine. However, during their clinic visits, patients with these “small” strokes often express feeling very fatigued, inattentive, unable to concentrate, cognitively slow, etc. While they may not have a visible disability, they still struggle to return to work and normal life due to this cognitive dysfunction.
In order to investigate cognition post-stroke, patients with relatively small strokes were enrolled in the “Recovery Study” at their first clinic visit. At each visit, the patient underwent a battery of cognitive testing that evaluated six domains, including: verbal memory, spatial memory, motor speed, processing speed, executive function, and global cognition.
This study found that cognitive impairment across multiple domains is common at 1-month following a minor stroke, regardless of location in the brain. These results suggest there is some sort of global cognitive network, and a minor stroke can cause a generalized disruption of that network.
These results also demonstrated that the average scores in every domain improved from the 1-month to 6-month follow-ups; however, while some patients continue to improve from 6- to 12-months, some patients’ scores plateau and even decrease. The lab is currently investigating that discrepancy, to identify the possible factors that drive continued improvement and potentially the factors that predict long-term decline.
Publication
Elisabeth B. Marsh, Sheena Khan, Rafael H. Llinas, Keenan A. Walker, Jason Brandt. Multi-domain cognitive dysfunction after minor stroke suggests generalized disruption of cognitive networks. Brain and Behavior 2022; DOI:10.1002/brb3.2571 Click to read article
Dallasta I, and Marsh EB. Poststroke Cognitive Decline: Is Functional Connectivity the Key to Tangible Therapeutic Targets? Stroke 2024 May;55(5). Click to read artice.
Scrambler Therapy
Scrambler therapy is a form of non-invasive pain treatment. It is a method of neuromodulation, which alters nerve activity by delivering electrical signals through electrodes on the skin. Using electrical impulses, Scrambler therapy can deliver “non-pain signals” to the brain along the same nerves that usually send the pain messages. Scrambler therapy was cleared by the US Food and Drug Administration in 2009. Scrambler therapy has been used in multiple conditions that cause neuropathic pain, that is pain that is caused by direct injury to the nerves. It can be used for acute or chronic pain.
Scrambler device. (A) The Scrambler device. (B) Electrode placement was individualized based on the reported area of pain.
Patients treated with Scrambler therapy:
• Pain caused by nerve damage from chemotherapy (neuropathy)
• Chronic pain due to cancer
• Pain from chronic conditions (MS, TM, DM, and schwannomatosis)
• Post-operative neuropathic pain
• Pain after stroke
• Postherpetic neuralgia (pain after shingles)
• Phantom limb pain
Scrambler therapy is designed to reprogram the pain system by stimulating the surface receptors of the C-fibers in the affected nerves. To achieve this, electrodes are placed surrounding the area of pain. The electrical stimulation reorganizes dysfunctional signaling, blocking pain signals. The brain receives the scrambled electrical stimulation and interprets it as normal, non-pain signal.
Publication
Robert Stowell-Campos, Erin Lawrence, Elisabeth Breese Marsh, Dawn Merbach. Scrambler Therapy for Treatment of Poststroke Pain. September, 2024. https://doi.org/10.1002/acn3.52201
Magnetoencephalography (MEG)
As part of our research, we are interested in higher level cognitive processes such as attention and multi-tasking. Even after small strokes, these activities can become impaired. This results in the inability for previously high-functioning individuals (school teachers, musicians, CEOs) to re-integrate into their prior home and workplace environments. It results in divorce, loss of jobs, and poor quality of life. The cognitive difficulties seem to occur regardless of the location of the stroke, and the underlying cause is poorly understood. It may be because the brain functions as a network (in other words, you require all of your brain to be functioning normally to be at your best). In order to determine if this is the case and how connections change after stroke, we are partnering with the University of Maryland to determine what is happening in the brain to impair cognition. Eligible patients with small strokes and difficulty with cognition on testing in our clinic travel to our partnering institute where they undergo magnetoencephalography (MEG). Similar to an MRI, the MEG records which areas of the brain are active during various activities. Testing is performed about 1 month after stroke and repeated at 6, 12, and 24 months. Our preliminary data are exciting! A 42-year-old executive presented to clinic with a small stroke, slow processing speed, and poor executive functioning that prohibited him from returning to work and leading meetings. The stroke itself did not explain his symptoms, but MEG showed diffuse abnormal activation within the frontal lobes, an important area for higher level processing (see left figure). These findings indicate that our hypotheses may be correct, but larger studies are needed. If we can determine the brain changes responsible for post-stroke cognitive impairment, we will be able to predict who is most likely to recover, devise better treatment strategies, and promote faster and fuller recovery after stroke.
Funding Source: American Heart Association
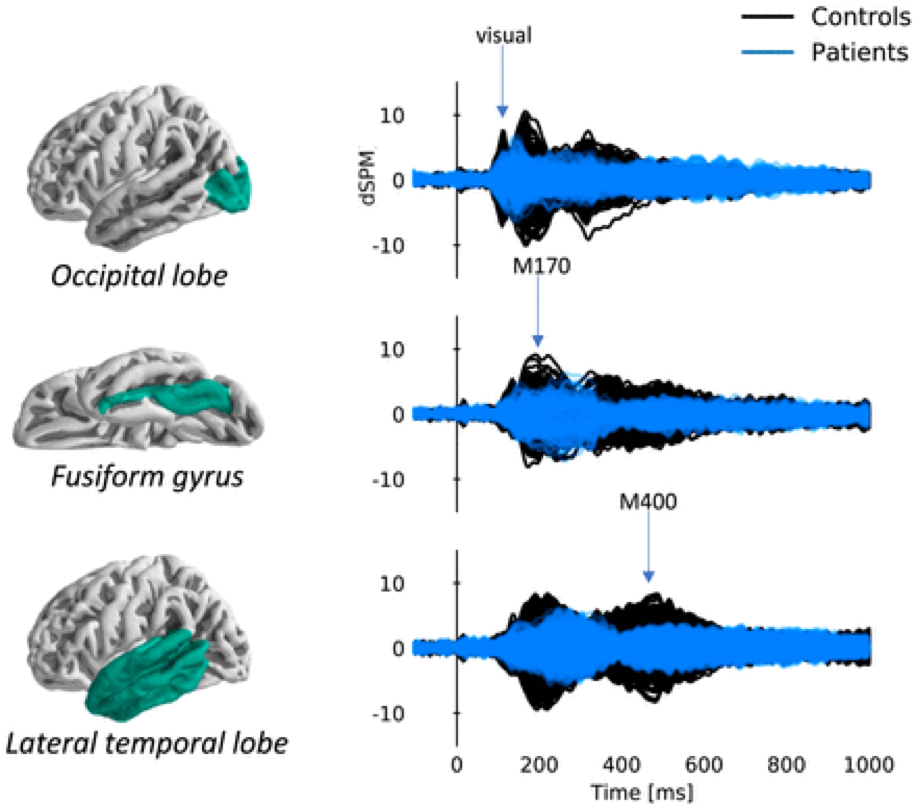
Our pilot MEG study is complete! We compared cerebral activation patterns for stroke patients during a word-picture matching task one month post-stroke compared to a group of age-matched controls and found decreased amplitude and temporal dispersion in the areas of the brain that are responsible for visual word processing. These results demonstrate that disruption of network dynamics may be responsible for difficulty with attention and concentration after stroke. These differences persisted 6 months after infarct, though clinical exams continued to improve, and we are currently bringing participants back to explore chronic changes, greater than 12 months post-stroke.
Publication
Elisabeth B. Marsh, Christian Brodbeck, Rafael H. Llinas, Dania Mallick, Joshua P. Kulasingham, Jonathan Z. Simon, Rodolfo R. Llinas. Proceedings of the National Academy of Sciences Dec 2020, 202013231; DOI: 10.1073/pnas.2013231117
Altered directional functional connectivity underlies post-stroke cognitive recovery
Small ischaemic strokes can result in cognitive deficits. After stroke, people show the most improvement in the first 6 months, but some continue to report disabling deficits after a year that can alter their lives and prevent them from recovering fully. These symptoms appear independent of lesion location, suggesting they arise from generalized disruption of cognitive networks. The mechanism by which many recover remains poorly elucidated. In addition, the longer-term trajectory of these patients is variable. Some continue to improve while others revert to worsened cognitive performance. The underlying neurophysiology warranted further investigation. Our pilot data strongly supported that altered functional connectivity may underlie cognitive deficits post-stroke so we subsequently designed and implemented a study using formal connectivity analyses.
For this study, we evaluated six patients with minor stroke exhibiting cognitive impairment 6–8 weeks post-infarct and four age-similar controls. Resting-state magnetoencephalography data were collected. Evaluations of both groups were repeated 6- and 12 months later. Our data shows that after stroke, inter-hemispheric connectivity between the frontoparietal cortex and the non-frontoparietal cortex significantly increased between visits 1 and 2, corresponding to uniform improvement in reaction times and cognitive scores. Initially, the majority of functional links originated from non-frontal areas contralateral to the lesion, connecting to ipsilesional brain regions. By visit 2, inter-hemispheric connections, directed from the ipsilesional to the contralesional cortex significantly increased. At visit 3, patients demonstrating continued favorable cognitive recovery showed less reliance on these inter-hemispheric connections. These changes were not observed in those without continued improvement. Our findings provide supporting evidence that the neural basis of early post-stroke cognitive dysfunction occurs at the network level, and continued recovery correlates with the evolution of inter-hemispheric connectivity.
Publication
Solemani B., Dallasta I., Das P., Kulasinham J.P, Girgenti, S., Simon J. Z., Babadi B., Marsh, E.B. Altered Directional Functional Connectivity Underlies Post-Stroke Cognitive Recovery. Brain Communications (2023). https://doi.org/10.1093/braincomms/fcad149
Potential Treatment, Mindfulness
Our MEG data shows that brain activation is slower and decreased in patients who have suffered minor strokes compared to controls. Many individuals suffering minor strokes report significant problems with concentration, attention, and mood, making it harder to return to their prior lifestyle. Problems returning to work or home can result in early retirement or loss of independence, especially in the older population. Unfortunately, as many patients do not qualify for rehabilitation after their strokes, there is a need to identify effective treatment options to improve recovery. Mindfulness training may be an attractive therapeutic option for improving recovery and helping individuals reintegrate into their prior home and workplace environments. A combination of meditation, body awareness, and yoga, Mindfulness Based Stress Reduction (MBSR) is an active process thought to engage the frontal lobes. MBSR has shown improved performance during tasks of executive function in patients with chronic stroke.
We are studying the effect of MBSR in the early phase of stroke recovery to see if this intervention can help prevent problems after strokes. Patients were enrolled and randomly assigned to either an 8-week course of MBSR or to the control treatment, a weekly Stroke Support Group (SSG). All participants underwent neuroimaging using MEG pre- and post-intervention to determine the neurophysiologic effect of treatment.
Our preliminary results show that there was more activity in the frontoparietal and default networks in the mindfulness group, receiving more input post-intervention from other brain regions. These results may have been affected by the level of engagement, which was a variable we collected and plan on looking into for secondary analyses. In addition, MBSR patients had better results in two of the tasks associated with the frontoparietal network that relies heavily on executive function. Our preliminary MEG results indicate that mindfulness has a greater effect on cognitive recovery and functional connectivity of minor stroke patients compared to a standard Stroke Support Group. Our analyses are ongoing.
Publications:
Girgenti S.; Dallasta I.; Lawrence E.; Merbach D.; Simon JZ.; Llinas R; Gould NF.; Marsh EB. Modified-Mindfulness Based Stress Reduction as a Treatment for Cognitive Recovery in Patients with Minor Stroke: a Randomized Controlled Trial (out for review).
Funding Source: National Institutes of Health
Transcranial Direct Current Stimulation (tDCS)
Small strokes can result in cognitive impairment. Small lesions, regardless of their location can lead to acute cognitive decline. Most people show improvement in the first 6 months post-stroke, but up to a third continue to report disabling deficits after a year. Persisting dysexecutive deficits can alter the lives of patients and prevent them from recovering fully, affecting quality of life. More effective treatments are necessary to help these patients with significant potential to recover fully.
Our preliminary data shows that the frontoparietal network (FPN), responsible for higher level cognitive tasks and executive function, is disrupted and leads to the clinical deficits observed. Our findings identify this as a novel therapeutic target for intervention. Transcranial direct current stimulation (tDCS) modulates cortical excitability and strengthens connectivity by producing and promoting facilitatory effects. This brain stimulation method is more effective when paired with a task that engages focal activation since it only induces firing neurons near threshold. Our study will look at the effectiveness of A-tDCS when combined with computerized cognitive therapy (CCT) to alter functional connectivity of the FNP. We plan to recruit 100 patients with minor stroke > 6 months post-infarct and randomize them to tDCS versus sham plus 15 sessions of cognitive therapy. We hypothesize that tDCS will augment connectivity of networks targeted during training (specifically the FPN) and that patients will show increased clinical improvement acutely following therapy that will last for months after treatment. Our pilot data suggest improvement in chronic deficits after treatment with tDCS and confirm alterations in the connectivity of the FPN. Along with clinical evaluation, we will use MEG to evaluate activation and connectivity within the FPN pre- and post-intervention to ensure target engagement.
Outcomes in Patients with Minor Stroke: Diagnosis and Management in the Post-thrombectomy Era
Thanks to the advances of mechanical thrombectomy and better preventative strategies, a higher number of patients are being discharged home from the hospital with the so-called minor strokes. This has significantly changed the landscape of stroke recovery. Unfortunately, while symptoms may be categorized as mild compared to individuals with higher NIH Stroke Scale scores, the physical, cognitive, and emotional sequelae can be disabling and result in failure to return to work and poor quality of life in a population with significant potential to recover fully. In this review, we discuss the current state of minor stroke, the most common pattern of resulting deficits, what is known about the underlying pathophysiology that leads to a relatively global pattern of impaired cognition following an infarct in any location, and special considerations for treatment based on this population’s unique needs. Raising awareness of the current morbidity associated with minor stroke, the need for a uniform definition that allows for comparisons of individuals across studies, and further research focused on this population to optimize outcomes, has the potential to significantly improve recovery.
Publication
Marsh, E.B., Girgenti, S., Llinas, E.J. et al. Outcomes in Patients with Minor Stroke: Diagnosis and Management in the Post-thrombectomy Era. Neurotherapeutics (2023). https://doi.org/10.1007/s13311-023-01349-5